Introduction
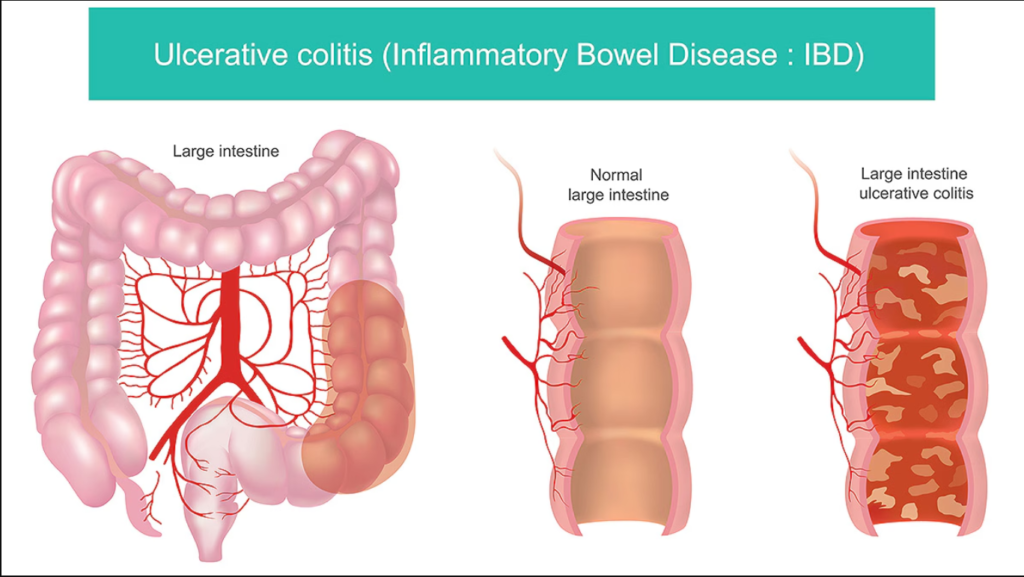
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the large intestine (colon) and rectum. Characterized by inflammation and ulceration of the intestinal lining, ulcerative colitis can cause significant discomfort and disrupt daily life. This article will explore the causes, symptoms, treatment options, and lifestyle management strategies for those living with ulcerative colitis, aiming to provide valuable insights and support for patients and their families.
What is Ulcerative Colitis?
Ulcerative colitis is a type of inflammatory bowel disease that causes long-lasting inflammation and ulcers in the digestive tract. It is distinct from Crohn’s disease, another form of IBD, which can affect any part of the gastrointestinal tract. Ulcerative colitis specifically targets the innermost lining of the colon and rectum.
The disease often manifests in episodes or flare-ups, where symptoms worsen, followed by periods of remission. The exact cause of ulcerative colitis remains unknown, but several factors may contribute, including genetics, the immune system, and environmental triggers.
Causes of Ulcerative Colitis
While the precise cause of ulcerative colitis is not fully understood, several factors are believed to play a role:
- Genetics: Individuals with a family history of ulcerative colitis or other inflammatory bowel diseases are at a higher risk of developing the condition. Specific genetic mutations may also increase susceptibility.
- Immune System: An abnormal immune response may contribute to the development of ulcerative colitis. The immune system may mistakenly attack healthy cells in the colon, leading to inflammation.
- Environmental Factors: Certain environmental factors, such as diet, pollution, and stress, may trigger or exacerbate ulcerative colitis symptoms. A diet high in processed foods and low in fiber has been associated with a higher risk of developing IBD.
- Microbiome Imbalance: The gut microbiome, which consists of trillions of microorganisms, plays a crucial role in digestive health. An imbalance in gut bacteria may influence the onset of ulcerative colitis.
Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis can vary widely among individuals and may change over time. Common symptoms include:
- Abdominal Pain and Cramping: Patients often experience discomfort or pain in the abdomen, which may be accompanied by cramping.
- Diarrhea: Frequent, loose stools are a hallmark symptom of ulcerative colitis. Patients may experience urgent bowel movements and may sometimes notice blood or mucus in their stool.
- Fatigue: Chronic inflammation and nutrient malabsorption can lead to fatigue and a general feeling of malaise.
- Weight Loss: Unintentional weight loss may occur due to decreased appetite, dietary restrictions, and nutrient malabsorption.
- Loss of Appetite: Many individuals with ulcerative colitis experience a reduced desire to eat, which can contribute to weight loss.
- Fever: Some patients may develop a low-grade fever during flare-ups.
- Anemia: Chronic blood loss from the intestines can lead to anemia, characterized by fatigue and weakness.
Symptoms can vary in severity, with some individuals experiencing mild discomfort while others may have debilitating symptoms that significantly impact their quality of life.
Diagnosis of Ulcerative Colitis
If ulcerative colitis is suspected, a healthcare provider will typically perform a thorough evaluation, which may include:
- Medical History: A detailed medical history will be taken, including information about symptoms, family history of IBD, and any previous gastrointestinal issues.
- Physical Examination: A physical exam may reveal signs of dehydration, abdominal tenderness, or other indicators of inflammation.
- Laboratory Tests: Blood tests may be conducted to check for anemia, signs of infection, or inflammatory markers. Stool tests can help rule out infections that may mimic ulcerative colitis.
- Endoscopy: A colonoscopy is often the primary diagnostic tool for ulcerative colitis. During this procedure, a thin, flexible tube with a camera is inserted through the rectum to visualize the colon and collect tissue samples (biopsies) for analysis.
- Imaging Studies: In some cases, imaging studies such as X-rays or CT scans may be ordered to assess the extent of inflammation and complications.
Treatment Options for Ulcerative Colitis
The management of ulcerative colitis aims to reduce inflammation, relieve symptoms, and maintain remission. Treatment options may include:
- Medications:
- Anti-Inflammatory Drugs: Aminosalicylates (e.g., mesalamine) are commonly used to reduce inflammation in the colon.
- Corticosteroids: These are used for short-term management of moderate to severe symptoms but are not recommended for long-term use due to potential side effects.
- Immunosuppressants: Medications that suppress the immune response (e.g., azathioprine, mercaptopurine) may be prescribed for individuals who do not respond to other treatments.
- Biologics: Targeted therapies, such as infliximab or adalimumab, may be used to treat moderate to severe ulcerative colitis by targeting specific pathways in the inflammatory process.
- Nutritional Support: A registered dietitian can help individuals with ulcerative colitis identify trigger foods and develop a balanced diet that minimizes symptoms. Some may benefit from a low-fiber diet during flare-ups to reduce bowel movements and discomfort.
- Surgery: In severe cases or when medical therapy fails, surgical intervention may be necessary. Surgery typically involves removing the colon (colectomy) and creating a new way for waste to exit the body. This can provide a permanent cure for ulcerative colitis.
- Lifestyle Modifications: Stress management techniques, regular exercise, and adequate sleep are important for managing ulcerative colitis. Many patients find that mindfulness practices, yoga, or counseling can help reduce stress, which may trigger flare-ups.
Living with Ulcerative Colitis
Living with ulcerative colitis can be challenging, but several strategies can help individuals manage their condition effectively:
- Regular Follow-Up: Routine check-ups with a healthcare provider are essential for monitoring disease progression and adjusting treatment as needed.
- Educate Yourself: Understanding ulcerative colitis and its management can empower individuals to make informed decisions about their health. Joining support groups or educational programs can provide valuable resources and a sense of community.
- Communicate Openly: Open communication with healthcare providers and loved ones about symptoms and treatment preferences can lead to better care and support.
- Keep a Symptom Journal: Tracking symptoms, dietary habits, and triggers can help identify patterns and potential flare-ups. This information can be valuable for discussions with healthcare providers.
- Seek Support: Emotional support from friends, family, or support groups can make a significant difference in coping with the challenges of living with ulcerative colitis. Connecting with others who understand the condition can provide comfort and practical advice.
Conclusion
Ulcerative colitis is a chronic condition that requires ongoing management and support. While the exact cause remains unclear, understanding the symptoms, treatment options, and lifestyle adjustments can empower individuals to lead fulfilling lives despite the challenges of this disease. If you suspect you may have ulcerative colitis or have been diagnosed, working closely with healthcare providers to develop a personalized treatment plan is crucial. With the right approach, individuals with ulcerative colitis can achieve remission and improve their quality of life.





