Introduction
Cardiovascular disease (CVD) encompasses a range of conditions affecting the heart and blood vessels, including coronary artery disease, heart attacks, stroke, and hypertension. CVD is one of the leading causes of morbidity and mortality worldwide, highlighting the need for awareness, early detection, and effective management. This article will explore the different types of cardiovascular disease, risk factors, symptoms, diagnostic procedures, treatment options, and preventive measures to promote cardiovascular health.
What is Cardiovascular Disease?
Cardiovascular disease refers to a group of disorders that affect the heart and blood vessels. These conditions can lead to serious complications, including heart attacks, strokes, and heart failure. The World Health Organization (WHO) estimates that CVD accounts for approximately 32% of global deaths each year, making it a critical public health issue.
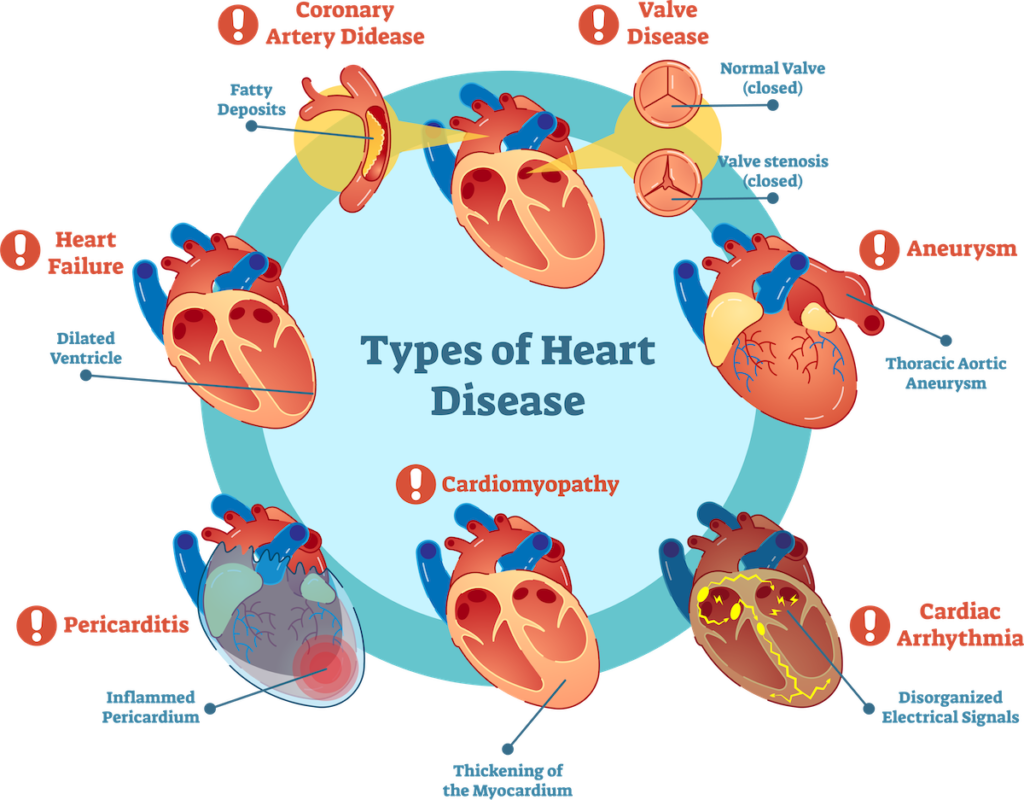
Types of Cardiovascular Disease
- Coronary Artery Disease (CAD): This is the most common type of CVD, characterized by the narrowing or blockage of coronary arteries due to atherosclerosis (the buildup of fatty deposits). CAD can lead to chest pain (angina) and heart attacks.
- Heart Attack (Myocardial Infarction): A heart attack occurs when blood flow to a part of the heart is blocked, causing damage to heart muscle. It is often the result of severe coronary artery disease.
- Stroke: A stroke occurs when blood flow to the brain is interrupted, either due to a blockage (ischemic stroke) or bleeding (hemorrhagic stroke). Both types can result in significant brain damage and disability.
- Hypertension (High Blood Pressure): Chronic high blood pressure can lead to various cardiovascular issues, including heart disease and stroke. It often goes unnoticed, earning it the title “silent killer.”
- Heart Failure: Heart failure occurs when the heart is unable to pump sufficient blood to meet the body’s needs. This can result from various underlying conditions, including CAD and hypertension.
- Peripheral Artery Disease (PAD): PAD affects blood flow to the limbs, usually due to atherosclerosis. It can cause pain and cramping in the legs and increase the risk of heart attacks and strokes.
- Arrhythmias: These are irregular heartbeats that can disrupt the heart’s ability to pump blood effectively. Some arrhythmias are harmless, while others can be life-threatening.
Risk Factors for Cardiovascular Disease
Understanding the risk factors for cardiovascular disease is crucial for prevention. Some risk factors are modifiable, while others are non-modifiable.
Non-Modifiable Risk Factors
- Age: The risk of CVD increases with age, particularly for men over 45 and women over 55.
- Gender: Men generally have a higher risk of CVD at a younger age compared to women, although the risk for women increases after menopause.
- Family History: A family history of heart disease or stroke can increase an individual’s risk, indicating a genetic predisposition.
Modifiable Risk Factors
- Unhealthy Diet: Diets high in saturated fats, trans fats, cholesterol, and sodium can contribute to obesity, hypertension, and atherosclerosis.
- Physical Inactivity: A sedentary lifestyle can lead to weight gain and increase the risk of high blood pressure, diabetes, and high cholesterol.
- Tobacco Use: Smoking damages blood vessels and accelerates the development of atherosclerosis, significantly increasing the risk of CVD.
- Excessive Alcohol Consumption: Heavy drinking can lead to high blood pressure, irregular heartbeats, and cardiomyopathy (heart muscle disease).
- Obesity: Excess body weight is linked to high blood pressure, diabetes, and elevated cholesterol levels, all of which contribute to cardiovascular disease.
- Diabetes: Individuals with diabetes have a higher risk of developing cardiovascular disease due to high blood sugar levels damaging blood vessels.
- Stress: Chronic stress may lead to unhealthy coping mechanisms, such as poor diet and smoking, which can contribute to CVD.
Symptoms of Cardiovascular Disease
Symptoms of cardiovascular disease can vary depending on the specific condition and may range from mild to severe. Some common symptoms include:
- Chest Pain or Discomfort: Often described as a feeling of pressure, squeezing, or fullness. This symptom may indicate angina or a heart attack.
- Shortness of Breath: Difficulty breathing may occur with exertion or at rest, signaling potential heart failure or other heart conditions.
- Fatigue: Unexplained fatigue, particularly in women, can be an early warning sign of heart disease.
- Palpitations: Irregular heartbeats or a racing heart may indicate an arrhythmia or other heart conditions.
- Swelling: Edema, or swelling in the legs, ankles, and feet, can occur in heart failure or other cardiovascular issues.
- Nausea or Indigestion: These symptoms, particularly when accompanied by chest discomfort, may indicate a heart attack, especially in women.
- Dizziness or Lightheadedness: These symptoms can occur due to reduced blood flow to the brain and may indicate serious cardiovascular problems.
Diagnosing Cardiovascular Disease
Accurate diagnosis is essential for effective management of cardiovascular disease. Healthcare providers utilize a variety of tests and procedures to evaluate cardiovascular health:
1. Medical History and Physical Examination
A thorough medical history and physical examination are the first steps in diagnosing CVD. The healthcare provider will assess risk factors, symptoms, and family history.
2. Blood Tests
Blood tests can help assess cholesterol levels, blood sugar levels, and other markers of cardiovascular health. Key tests include:
- Lipid Profile: Measures total cholesterol, LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides.
- Blood Glucose Test: Assesses blood sugar levels to identify diabetes or prediabetes.
3. Electrocardiogram (ECG or EKG)
An ECG records the electrical activity of the heart and can help identify arrhythmias, heart attacks, and other heart conditions.
4. Echocardiogram
This ultrasound test uses sound waves to create images of the heart’s structure and function, helping to assess heart size, shape, and pumping ability.
5. Stress Testing
Stress tests evaluate how the heart performs during physical activity. They can help identify coronary artery disease and assess exercise capacity.
6. Cardiac Catheterization
In this invasive procedure, a thin tube is inserted into a blood vessel to visualize the coronary arteries and assess blood flow. It can also be used to perform angioplasty.
7. CT or MRI Scans
Advanced imaging techniques like computed tomography (CT) or magnetic resonance imaging (MRI) may be used to evaluate heart and blood vessel structures in detail.
Treatment Options for Cardiovascular Disease
The treatment of cardiovascular disease varies based on the specific condition, severity, and individual patient needs. Common treatment options include:
1. Lifestyle Modifications
Making healthy lifestyle changes is a foundational aspect of managing cardiovascular disease. Recommended modifications include:
- Healthy Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage weight and lower cholesterol and blood pressure.
- Regular Exercise: Engaging in regular physical activity (at least 150 minutes of moderate exercise per week) can improve cardiovascular health and reduce the risk of complications.
- Weight Management: Achieving and maintaining a healthy weight can reduce the risk of CVD and improve overall health.
- Smoking Cessation: Quitting smoking significantly reduces the risk of cardiovascular disease and improves heart health.
- Stress Management: Techniques such as mindfulness, yoga, and regular relaxation can help manage stress levels.
2. Medications
Several medications are commonly prescribed to manage cardiovascular disease and its risk factors:
- Antihypertensives: These medications help lower blood pressure, reducing strain on the heart and blood vessels.
- Statins: Statins lower cholesterol levels and reduce the risk of heart attack and stroke.
- Antiplatelet Agents: Medications like aspirin prevent blood clots, lowering the risk of heart attack and stroke.
- Beta-Blockers: These medications reduce heart rate and blood pressure, helping to manage angina and heart failure.
- Diuretics: Also known as “water pills,” these help reduce fluid buildup and lower blood pressure.
3. Interventional Procedures
For more severe cases of cardiovascular disease, interventional procedures may be necessary:
- Angioplasty and Stenting: These procedures involve using a balloon to widen narrowed arteries and placing a stent to keep them open.
- Coronary Artery Bypass Grafting (CABG): CABG is a surgical procedure that reroutes blood flow around blocked coronary arteries.
- Heart Valve Repair or Replacement: Surgery may be necessary to repair or replace damaged heart valves.
- Pacemaker or Implantable Cardioverter-Defibrillator (ICD): These devices regulate heart rhythm and prevent life-threatening arrhythmias.
4. Cardiac Rehabilitation
Cardiac rehabilitation is a structured program designed to help individuals recover from heart-related conditions. It typically includes:
- Supervised Exercise: A tailored exercise program to improve cardiovascular fitness.
- Education: Information on heart-healthy living, nutrition, and managing stress.
- Support: Counseling and support groups to help patients cope with the emotional aspects of cardiovascular disease.
Preventing Cardiovascular Disease
Prevention is key to reducing the risk of cardiovascular disease. By adopting a proactive approach, individuals can significantly lower their risk factors:
1. Regular Health Screenings
Routine check-ups and screenings for blood pressure, cholesterol, and blood sugar levels can help identify potential risk factors early.
2. Healthy Eating Habits
Emphasizing a heart-healthy diet can significantly impact cardiovascular health. Consider the following dietary tips:
- Focus on Fruits and Vegetables: Aim for at least five servings of fruits and vegetables daily to provide essential vitamins and minerals.
- Choose Whole Grains: Whole grains like brown rice, quinoa, and whole wheat bread are rich in fiber and help maintain healthy cholesterol levels.
- Limit Saturated and Trans Fats: Reduce the intake of processed foods, fried foods, and fatty cuts of meat to lower cholesterol levels.
- Reduce Sodium Intake: Limiting salt intake can help manage blood pressure. Aim for less than 2,300 mg of sodium per day.
3. Stay Physically Active
Engaging in regular physical activity is crucial for maintaining a healthy heart. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week.
4. Maintain a Healthy Weight
Achieving and maintaining a healthy weight through diet and exercise can significantly lower the risk of cardiovascular disease.
5. Limit Alcohol Consumption
If you choose to drink alcohol, do so in moderation. For women, this means up to one drink per day, and for men, up to two drinks per day.
6. Manage Stress
Practicing stress management techniques, such as meditation, yoga, or deep-breathing exercises, can help lower blood pressure and improve heart health.
7. Quit Smoking
Quitting smoking is one of the most significant steps an individual can take to reduce the risk of cardiovascular disease. Seek support through counseling or smoking cessation programs.
Conclusion
Cardiovascular disease remains a leading global health concern, but many of its risk factors are modifiable. By understanding the various types of CVD, recognizing risk factors, and implementing preventive measures, individuals can significantly reduce their risk of developing cardiovascular disease.
Regular health screenings, a heart-healthy lifestyle, and adherence to medical advice are essential in managing cardiovascular health. Whether through lifestyle modifications, medications, or interventional procedures, proactive measures can lead to improved outcomes and enhanced quality of life for those affected by cardiovascular disease.
If you or a loved one is at risk for cardiovascular disease or experiencing symptoms, it’s crucial to consult a healthcare professional for evaluation and personalized care. With awareness and appropriate action, we can combat cardiovascular disease and promote a healthier future for ourselves and our communities.





