Introduction
Pneumonia is a serious respiratory condition that affects millions of people worldwide. Characterized by inflammation of the air sacs in one or both lungs, pneumonia can cause a range of symptoms, from mild to severe. Understanding pneumonia is crucial for early detection and effective management. In this article, we will explore the different types of pneumonia, their causes, symptoms, diagnostic methods, treatment options, and preventive measures.
What is Pneumonia?
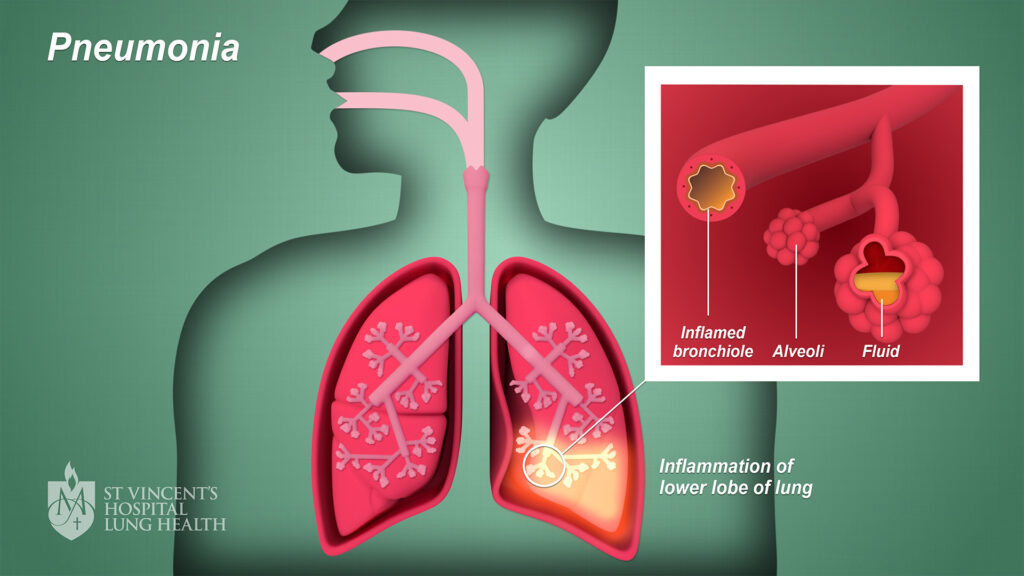
Pneumonia is an infection that inflames the air sacs in the lungs, known as alveoli. These air sacs may fill with fluid or pus, leading to symptoms such as cough, fever, chills, and difficulty breathing. Pneumonia can be caused by various pathogens, including bacteria, viruses, and fungi.
Types of Pneumonia
Pneumonia can be classified based on various criteria:
- By Cause:
- Bacterial Pneumonia: Often caused by bacteria such as Streptococcus pneumoniae, this type can develop on its own or after a cold or flu.
- Viral Pneumonia: Commonly caused by viruses like influenza or respiratory syncytial virus (RSV), viral pneumonia is typically less severe than bacterial pneumonia.
- Fungal Pneumonia: Caused by fungi, this type is more common in individuals with weakened immune systems and can result from inhaling fungal spores.
- By Setting:
- Community-Acquired Pneumonia (CAP): Acquired outside of healthcare settings, CAP is the most common type of pneumonia.
- Hospital-Acquired Pneumonia (HAP): This type occurs during a hospital stay, usually after 48 hours of admission, and is often more serious due to the presence of antibiotic-resistant bacteria.
- Ventilator-Associated Pneumonia (VAP): A type of HAP that develops in people who are on mechanical ventilation.
- By Severity:
- Mild Pneumonia: Often treated at home, mild pneumonia may cause manageable symptoms.
- Severe Pneumonia: Requires hospitalization, severe pneumonia can lead to significant health complications, especially in vulnerable populations.
Symptoms of Pneumonia
Pneumonia symptoms can vary based on the type of pneumonia, age, and overall health. Common symptoms include:
- Cough: This may produce phlegm, which can be green, yellow, or even blood-streaked.
- Fever: A high fever is common, along with chills and sweating.
- Shortness of Breath: Patients may experience difficulty breathing or a feeling of breathlessness.
- Chest Pain: This may worsen with deep breaths or coughing.
- Fatigue: Many individuals feel unusually tired or weak.
- Confusion: Especially in older adults, confusion or changes in mental awareness may occur.
Recognizing Severe Symptoms
While many cases of pneumonia are manageable at home, some symptoms require immediate medical attention:
- Rapid Breathing: Increased respiratory rate may indicate severe pneumonia.
- Blue Tint to Lips or Face: This can indicate low oxygen levels.
- High Fever: A persistent high fever (over 102°F or 39°C) may suggest a serious infection.
- Severe Chest Pain: Intense pain may signal complications such as pleurisy.
Causes of Pneumonia
Pneumonia can result from various pathogens. Here’s a closer look at the causes:
1. Bacteria
Bacterial pneumonia is typically caused by:
- Streptococcus pneumoniae: The most common bacterial cause of pneumonia in adults.
- Haemophilus influenzae: More common in those with underlying lung disease.
- Mycoplasma pneumoniae: Often causes atypical pneumonia, especially in younger individuals.
2. Viruses
Viral pneumonia can result from:
- Influenza Virus: Common in seasonal outbreaks and can lead to secondary bacterial infections.
- Respiratory Syncytial Virus (RSV): Particularly affects infants and young children.
- SARS-CoV-2: The virus responsible for COVID-19 can cause viral pneumonia.
3. Fungi
Fungal pneumonia is caused by:
- Histoplasma capsulatum: Found in areas with bird or bat droppings.
- Coccidioides immitis: Common in certain regions of the United States and can cause valley fever.
4. Aspiration
Aspiration pneumonia occurs when food, drink, or vomit is inhaled into the lungs, leading to infection. This is more likely in individuals with swallowing difficulties or reduced consciousness.
Risk Factors for Pneumonia
Certain groups are at higher risk for developing pneumonia, including:
- Age: Children under 2 and adults over 65 are more susceptible.
- Chronic Diseases: Conditions like asthma, COPD, diabetes, and heart disease can increase the risk.
- Weakened Immune System: Individuals with compromised immune systems, due to conditions like HIV/AIDS or treatments like chemotherapy, are more vulnerable.
- Smoking: Tobacco smoke damages lung tissue and reduces the ability to fight infections.
- Hospitalization: Being in a healthcare setting, especially with ventilators, raises the risk of HAP and VAP.
Diagnosing Pneumonia
Prompt and accurate diagnosis is essential for effective treatment. Healthcare providers use several methods to diagnose pneumonia:
1. Medical History and Physical Examination
A detailed medical history and physical examination are the first steps. The healthcare provider will ask about symptoms, recent illnesses, and any risk factors.
2. Chest X-ray
A chest X-ray is a crucial diagnostic tool that helps visualize the lungs and identify areas of infection or inflammation.
3. Blood Tests
Blood tests can help determine the type of infection (bacterial or viral) and assess overall health. A complete blood count (CBC) can show white blood cell levels, indicating infection.
4. Sputum Culture
Collecting sputum (mucus) for analysis can help identify the specific pathogen causing pneumonia. This is especially useful for determining appropriate antibiotic treatment.
5. Pulse Oximetry
This non-invasive test measures the oxygen saturation in the blood, helping to assess how well the lungs are functioning.
6. CT Scan
In complex cases, a CT scan can provide more detailed images of the lungs, helping to identify complications or other underlying issues.
Treatment Options for Pneumonia
Treatment for pneumonia varies based on the type, severity, and underlying health of the patient. Here’s a breakdown of common treatment options:
1. Antibiotics
Bacterial pneumonia is typically treated with antibiotics. The choice of antibiotic depends on the bacteria suspected or confirmed and the patient’s medical history.
2. Antiviral Medications
For viral pneumonia caused by influenza or other viruses, antiviral medications may be prescribed, particularly if started early in the course of the illness.
3. Fungal Treatments
Fungal pneumonia is treated with antifungal medications. The specific drug will depend on the type of fungus involved.
4. Supportive Care
In addition to medications, supportive care is vital:
- Rest: Adequate rest helps the body recover.
- Hydration: Drinking plenty of fluids helps thin mucus and keeps the body hydrated.
- Over-the-Counter Pain Relievers: Medications like ibuprofen or acetaminophen can help relieve pain and reduce fever.
5. Hospitalization
Severe cases of pneumonia may require hospitalization for close monitoring and advanced treatments, including:
- Intravenous (IV) Antibiotics: For serious infections that need aggressive treatment.
- Oxygen Therapy: To maintain adequate oxygen levels in the blood.
- Mechanical Ventilation: In critical cases where breathing support is necessary.
Complications of Pneumonia
While many cases of pneumonia are treatable, complications can arise, especially in high-risk individuals. Potential complications include:
- Pleural Effusion: Fluid accumulation in the pleural space surrounding the lungs, which may require drainage.
- Lung Abscess: A pus-filled cavity in the lung that may require antibiotics or surgical drainage.
- Sepsis: A life-threatening response to infection that can result in tissue damage and organ failure.
- Respiratory Failure: Severe pneumonia can impair lung function, requiring mechanical ventilation.
Preventing Pneumonia
Prevention is key to reducing the risk of pneumonia. Here are effective strategies:
1. Vaccination
Vaccination is one of the most effective ways to prevent pneumonia. Recommended vaccines include:
- Pneumococcal Vaccines: Protect against Streptococcus pneumoniae.
- Influenza Vaccine: Reduces the risk of viral pneumonia related to the flu.
2. Practice Good Hygiene
- Handwashing: Regularly washing hands can help prevent the spread of infections.
- Avoiding Close Contact: Stay away from individuals who are sick, especially during cold and flu season.
3. Quit Smoking
If you smoke, seek support to quit. Avoiding tobacco significantly lowers the risk of respiratory infections.
4. Healthy Lifestyle
- Balanced Diet: Eating a diet rich in fruits, vegetables, and whole grains supports a healthy immune system.
- Regular Exercise: Physical activity can improve lung function and overall health.
- Adequate Sleep: Prioritize good sleep hygiene to support immune function.
5. Manage Chronic Conditions
If you have chronic diseases, work with your healthcare provider to manage them effectively, reducing the risk of pneumonia.
Conclusion
Pneumonia is a significant health concern that can affect anyone, but understanding the symptoms, causes, and preventive measures can make a difference. Early detection and appropriate treatment are crucial for recovery, especially in vulnerable populations.
By taking proactive steps, such as vaccination, practicing good hygiene, and maintaining a healthy lifestyle, individuals can reduce their risk of pneumonia. If you or someone you know experiences symptoms of pneumonia, seek medical attention promptly to ensure a swift and effective response.
As awareness of pneumonia increases, so does the potential for prevention and better health outcomes for all.





